|
RESEARCH DEVELOPMENT Kurt Grey Physiotherapist |
PALPATION OF TISSUE THICKNESSA prerequisite when determining the ultrasound intensity in human tissue |
||||||||||||||||||||||||||||||||||||||
|
Main Menu:
ULTRASOUND Research and Development:
Clinical guidance Tools and Tutorials:
MISCELLANEOUS:
LINKS Contact:
Downloads:
Latest update : 23-03-2011
|
A FULL-TEXT REPORTGrey, K: Palpation of the thickness of the irradiated tissue in ultrasound treatment. 1992. A pilot study of the accuracy by simulation.
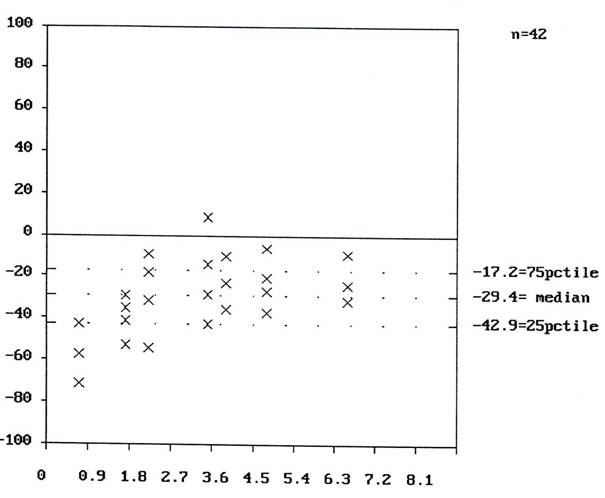
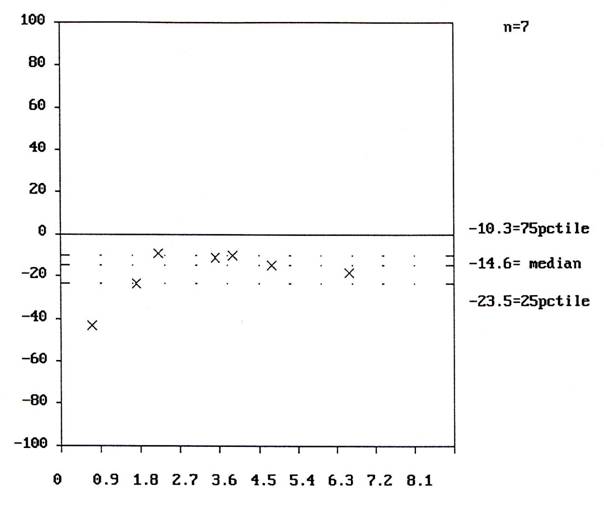
Graphics: Fig 1. Model and test points, drawing Fig 2. The probe, drawing Fig 3: Palpation, diagram of results Fig 4: Probe, diagram of results
In order to test the usefulness of palpation in determining the thickness of tissue, six physiotherapists simulated 42 measurements by palpation on models made out of foam rubber. All the physiotherapists underestimated the dimensions. There was a difference between palpation and control readings with a median of -0.7 cm (lower quartile = -1.2 cm, upper quartile = -0.5 cm) or 29 % (l.q. =-43%, u.q. = -17%), p < 0.00001. Measurements made with a probe showed a median difference of -0.4 cm or 15% (l.q. = -0.7 cm, u.q. = -0.3 cm). n=7. p= 0.0156. A compression of the foam rubber takes place at the tip of the palpating finger and the probe, but the compressed material still has some volume, which is probably the most important factor in the demonstrated underestimation. It seems that palpation can give a valuable estimate of the thickness of tissue if proper correction is made to compensate for the systematic error. Further investigation is necessary to determine the size of these errors in human tissue.
AcknowledgementsI wish to thank the participating physiotherapists from Aalborg Hospital. Morten Christensen and his colleagues from the hospitals Technical Dep. for providing the measuring probe, which they manufactured for this purpose. The project was supported by grants from "Danske fysioterapeuters Forskningsfond", and "Den Lægevidenskabelige Forskningsfond i Nordjyllands Amt". BACKGROUNDIn order to increase the reproducibility of therapeutic intensity the loss of energy due to attenuation must be calculated (1). The transformation of the intensity from the apparatus to the intensity at the site of the lesion is determined by the type and dimension of the tissue separating the skin surface and the lesion. A reliable measure of the distance between the skin surface and the target tissue (the lesion) is necessary for this purpose. An important measure is also the distance to the underlying bone, as this provides a prediction of the reflected ultrasound. The distance between surface and lesion can also play a role in the estimate of dynamic focusing and defocusing due to treatment on a curved surface. (See elsewhere on this homepage). In this project palpation as a means of measuring tissue dimensions is investigated.
PURPOSE The project evaluates the accuracy of palpation as a method for measuring tissue thickness. Practical issues of this method will be evaluated as well.
While this method would preferably be performed on humans and compared to scanning readings, this inexpensive pilot project was performed on models to explore the basic problems of the technique. Two models with a total of 7 measuring points (“test”) were manufactured for the project. The measuring points were meant to mimic palpation of the skin-bone distance. The models consisted of two wooden boxes (fig.1). Pieces of wood would mimic protruding bone. The boxes were filled with rubber foam and covered with several layers of foam, a rubber membrane and on top a 2 mm-layer of felt. This would act as “soft-tissue”. The therapists were instructed to estimate by palpation the distance from the felt-layer to the wooden ”bone”-protuberances. (Fig 1). Measurements of the distance from the wooden pieces to the top of the box with a ruler served as the ”true readings”.
A measuring probe (fig 2) was used to read the distance from ”skin” to ”bone” in a similar manner. The probe base is placed in contact with the surface. The central rod is then pushed into the “soft tissue”, compressing it until a “bony”, firm end feeling is met. The central rod is fixed with a screw. The depth is read on the scale on the rod. 6 physiotherapists each made 7 palpations on the models, - a total of 42 palpations. One therapist used the probe on the seven measuring points. The readings were in mm. The absolute and relative difference between the palpations and the “true readings” were calculated and tested with Wilcoxon-Pratt's test for paired data. The level of significance = 0.05.
RESULTSBy subtracting the ”depth by palpation” from the ”true reading” the misreading is calculated. If for example the distance measured by ruler is 1.5cm, and the therapist arrives at 1.3cm by palpation, the underestimate is 0.2 cm. In table I underestimation is shown by negative numbers. The difference between palpation and the ”true reading” was 29% (p<0.00001), and for the probe the difference was 15% (p=0.016). The results are displayed graphically in fig 3 and 4.
TABLE I. In this table the median difference between the palpation and ruler readings for each therapist is shown. The total is seen below and finally the median difference for the probe is listed.
Every participant underestimated the ”tissue thickness”. The average underestimation was 0.7 cm or 29 %. I found two sources explaining this. The foam rubber although compressed is not without extension, and should be considered larger than zero. This is true for palpation and the probe as well. Maybe the therapist overlooked the first soft pressure into the skin. The difference between palpation and probe is 14%, which could be accounted for by this explanation. It should, though, be considered that the ultrasound transducer often is pressed somewhat into the soft tissue during treatment, thereby reducing the distance from skin to lesion. The relative underestimate is largest by small depth. This is important since reflexion is larger, when bone is close to the transducer, and a reflexion-loop is possible between bone and transducer/air (re-reflexion…). The foam-cell were destroyed and deflated during the repeated compression. Larger series were thus not possible.
EXTERNAL VALIDITY The similarity between the models used in this investigation and human tissue is questionable. Human tissue must be expected to present a variety of density, viscosity, hydration, temperature etc resulting in a large variety of tissue flexibility. If results from human tissue were available, the method would seem simple. If the underestimate is 33% of the true value, the depth must be calculated after palpation, e.g. 2.2 cm by palpation equals 3.3 cm tissue depth. The method of this investigation only tested the "skin-bone" distance. Results for the equally relevant skin-lesion distance remains unclear. Larger variation must be expected since the bony end-feel is absent.
Palpation seems to be a useful tool in determining tissue thickness. The estimate of ”tissue” compression cannot be derived from the present investigation, but must be established in testing on humans. The probe yielded more stable results than digital palpation with less variation and less systematic error.
- o - |
||||||||||||||||||||||||||||||||||||||